Thesis: Obesity and undernutrition now exist side-by-side—in the same countries, cities, and even homes. There is no single fix. The answer is a fair, healthy, affordable food system, paired with respectful care, not stigma.
Syllabus: Public health(GS3), Food Security(GS3), Equity(GS2 & GS4), Human rights(GS2), Essay
Why now
New global updates show that, for the first time, more school-age children are overweight than underweight. Yet hundreds of millions still face hunger. India’s own surveys tell the same story: rising overweight/obesity across ages, while stunting and wasting persist in many districts. Interest in new GLP-1 drugs is surging, but prices and supply raise sharp equity questions.
Recent Data:
- Global (2022): ~2.5 billion adults overweight; ~890 million living with obesity (WHO, May 2025).
- Children (5–19) 2022: about 1 in 5 overweight; 1 in 10 underweight (UNICEF, Sep 2025).
- India (NFHS-5, 2019–21): 24% women and 23% men overweight/obese; under-5 overweight up to 3.4%.
- Hunger (2024): 638–720 million people faced hunger worldwide (SOFI, Jul 2025).
- GLP-1 stands for Glucagon-like peptide-1. It is a naturally occurring hormone produced in the intestine that helps regulate blood sugar levels by stimulating insulin release, inhibiting glucagon secretion, slowing digestion, and reducing appetite.
Put simply: the world is fighting too little food and too much unhealthy food at the same time.
Core Question & Context
The paradox is the double burden of malnutrition: undernutrition (stunting, wasting, micronutrient gaps) and over-nutrition (overweight/obesity and diet-related NCDs). It often shows up inside the same household. A parent may gain weight on cheap ultra-processed snacks while a child is stunted for lack of protein and micronutrients. This is not contradiction—it is what happens when calories are cheap, nutrients are costly, and daily life is more sedentary.
This shift did not happen overnight. Two long transitions converged.
- First, the nutrition transition: markets flooded the globe with refined carbs, sugary drinks, and aggressively marketed packaged foods.
- Second, the work-and-city transition: more screens and traffic, fewer safe parks and pavements, uneven access to safe water and fresh food. Together they create obesogenic environments, even where incomes are low.
India sits right in the middle of this change. Gains against undernutrition are too slow, while overweight rises among children, adolescents, and adults.
- Calling this a matter of “willpower” misses the point. Prices, marketing, infrastructure, and access to care tilt the field.
- New GLP-1 medicines genuinely help some people with obesity. But they cannot by themselves fix food deserts, aggressive marketing, or poverty. Drugs can help some; systems help everyone.

GLP 1 Uses
We need to tackle Hunger, Malnutrition and Obesity
The right approach is to do both: give strong clinical care to those who need it, and set food rules that make healthy options easier and cheaper for everyone.
- At the clinical level, treating obesity as a chronic disease saves lives and money.
- For high-risk patients, structured nutrition support, activity plans, counselling, GLP-1 therapy, and bariatric surgery reduce complications and hospitalisations.
- Ignoring care because “food environments are the root cause” is no kindness to those already unwell.
At the system level, smart regulation changes the default.
- Front-of-pack warning labels, strong school food standards, and limits on child-targeted marketing work quietly in the background, nudging behaviour without blaming people.
- Public programmes—mid-day meals, ICDS, and local procurement—can inject protein (pulses, eggs, dairy), millets, fruits, and vegetables into daily diets, lowering undernutrition and over-nutrition together.
- District dashboards that track stunting, anaemia, overweight, and food prices help tailor menus, subsidies, and farm support to local needs.
Justice has its own hard arithmetic. The right to food and right to health are not empty slogans; they form a baseline for policy. If healthy calories cost more than junk calories, rules must reshape markets—not just preach to families.
But it’s my Right to Eat
Single tools—whether pills or one big tax—cannot solve a system problem on their own. If policies ignore equity, rights, or supply chains, they backfire.
Medicines without diet and follow-up will disappoint; high prices and limited supply widen health gaps. A poorly designed sugary-drink tax may burden small vendors and low-income consumers if there are no affordable alternatives and no support to switch. Bans and warnings mean little where fresh food is scarce or unsafe. Without cold chains, clean water, and local markets, families simply cannot change.
- Stigma and Human Dignity
Shaming people for their body size or food choices not only hurts dignity but also keeps them away from medical care. Treating health as a human right means services must be respectful, safe, and accessible, so that people actually use them. - Corporate Resistance and Policy Gaps
Food companies often use advertising and lobbying to delay or weaken rules on food labels, school nutrition, and junk-food ads. To counter this, governments need to set strong rules, monitor compliance, and publish results so that public health goals are not compromised by private interests. - Global Inequality in Food and Health
Rich countries spend more on costly obesity drugs like GLP-1, even as the world wastes 1.05 billion tonnes of food in 2022 (about 132 kg per person). Meanwhile, 673 million people faced hunger in 2024. This shows a deep gap—some societies treat excess with expensive medicine, while others struggle with empty plates. - The Justice Question
The key issue is about priorities: Should global rules make it easier to access vaccines and pulses instead of sugary drinks? Should trade and marketing stop spreading ultra-processed foods in poor countries where even clean water and basic healthcare are missing? These choices represent the policy frontier of food and health justice today.
Way forward
There is no magic pill for solving hunger, obesity, or malnutrition. But we can take a clear, step-by-step path that works at different levels—government, markets, communities, and the global system. Each step must be simple, written, and time-bound.
1. Government: Build a Healthy Food Environment
- Make healthy the easy choice: front-of-pack warnings; strict school and anganwadi food standards; limits on junk-food marketing to children.
- Lower costs of healthy staples: reduce GST/levies on pulses, millets, eggs, fruits, vegetables; support local procurement so farmers benefit too.
- Use tax revenues wisely: earmark sugary-drink tax money for school meals, safe water, and play spaces.
- Invest in basics: safe water, sanitation, cold chains to reduce infections, spoilage, undernutrition, and obesity.
- Measure and adjust: track stunting, anaemia, overweight, and food prices with district dashboards; review quarterly.
2. Markets and Health System: Treat and Prevent Together
- Primary care services: nutrition advice, growth monitoring, timely referrals, plus mental-health and addiction support.
- Access to treatment: affordable programmes for GLP-1 drugs where needed, combined with lifestyle support.
- Industry responsibility: reformulate products with less salt, sugar, and trans-fat.
- Retail environment: place healthy staples at eye-level, not hidden.
- Employers and cities: provide healthy workplace meals, active breaks, safe walking/cycling routes, more parks.
3. Communities and Citizens: Dignity, Not Stigma
- Rights, not perks: affordable nutritious food and basic healthcare treated as entitlements.
- Local actions: kitchen gardens, millet and pulse recipes in schools, cooking demos, women’s collectives for local supply.
- Food literacy: teach families to read labels; explain ultra-processed foods without blame.
- Respectful care: stop weight-based teasing in schools/workplaces; ensure clinics use non-judgmental language.
4. International: Align Trade, Aid, and Standards
- Fair rules: stop rewarding empty calories while pricing out nutrients.
- Protect children: enforce global standards for labelling and marketing limits.
- Finance priorities: direct more funds to school meals, fortification, clean water, sanitation, and small farmers.
- Data and access: share open data on obesity drugs and prices; prevent rich-poor divides in access.
- Global fairness: if we can lower the cost of phones, we should lower the cost of pulses and healthy food.
5. Ethics Lens
- Justice: can the poorest really access healthy food and care?
- Utility and precaution: focus on basics like water and protein before expensive drugs.
- Dignity and rights: reject stigma; make the right to food and health real.
- Inter-generational fairness: today’s food system must not trap children in lifelong disease.
Exam hooks
Key takeaways
The double burden is real: undernutrition and obesity live side-by-side, so policy must tackle both. Systems, not slogans: labels, sch ool standards, affordable proteins, and safe water shift behaviour for everyone; medicines help some, systems help all. Equity first: design taxes and subsidies to protect low-income groups; guarantee access to care and healthy food where the need is greatest.
Mains question:
Explain why obesity and undernutrition co-exist in India and globally.
Hints: Frame a rights-based, equity-focused roadmap that balances clinical care with food-system reform, and reflect on the ethics of high-cost treatments in rich nations versus food shortages elsewhere.”
One-line wrap: Fix the food environment, protect rights, and use medicine wisely—that is how we beat hunger and obesity together.
Share This Story, Choose Your Platform!
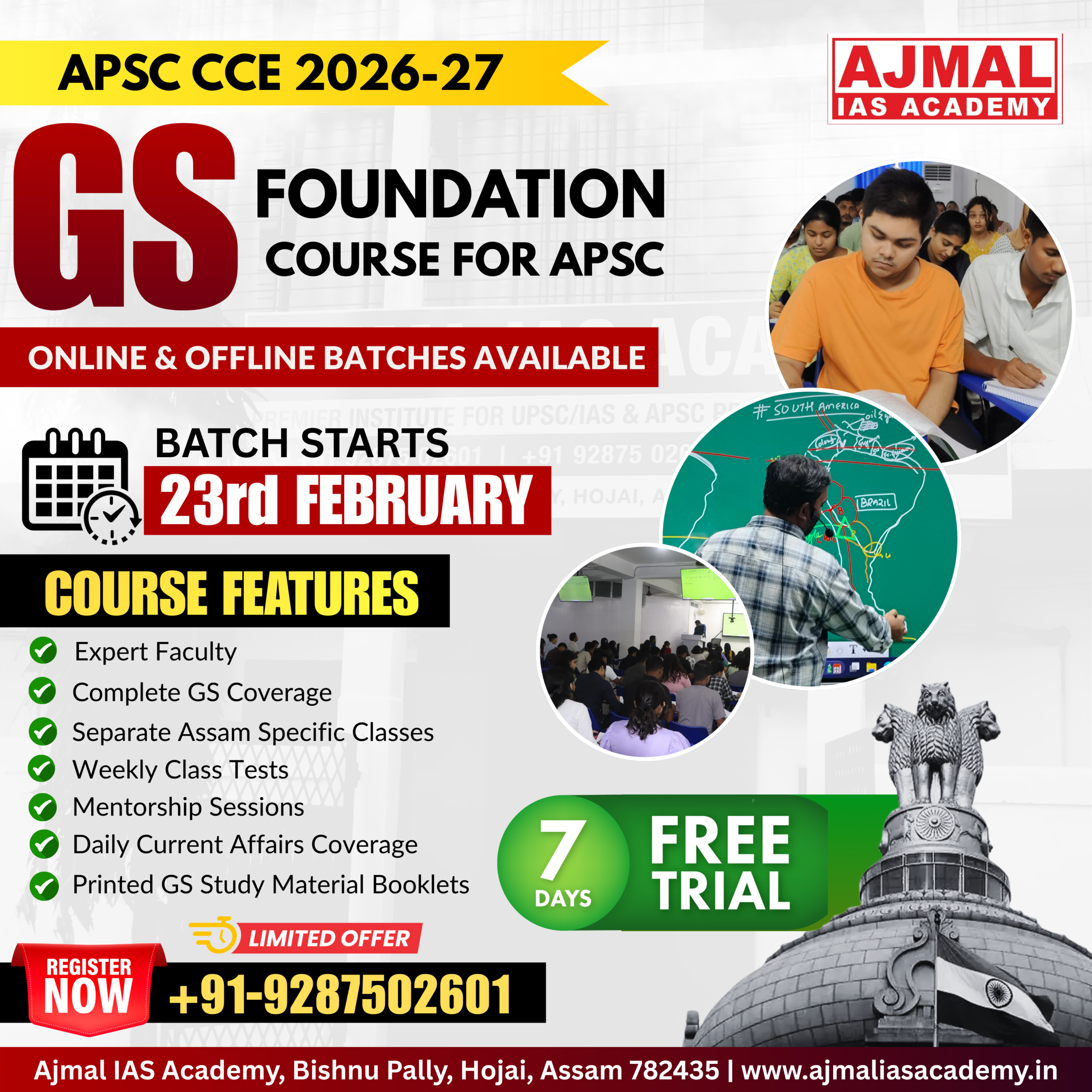
Start Yours at Ajmal IAS – with Mentorship StrategyDisciplineClarityResults that Drives Success
Your dream deserves this moment — begin it here.