Health Sector, Science and Technology, Social Justice, Governance, Pandemic & Disaster Management, and Current Affairs.
Many people who recovered from COVID show stiffer arteries than those who never had it—especially women. The effect is roughly like being five to ten years older in the blood vessels. Stiff arteries are silent but raise the chance of stroke, heart attack, kidney strain, and memory problems over time. With hundreds of millions of survivors worldwide, even a small extra risk can add up unless we act early.
What “stiff arteries” means: what the study saw, and why it matters
- Arterial stiffness means arteries lose their spring. The heart pushes harder, blood pressure tends to climb, and small vessels in the brain and kidneys get damaged more easily.
- Doctors often measure stiffness by pulse wave velocity—how fast the pressure wave from each heartbeat moves along a main artery. Faster speed = stiffer vessel.
A large multinational programme tracked about 2,400 people in over 18 countries. It compared those who had recovered from COVID with those who never had it, using standard measures of stiffness and blood pressure.
Patterns that stood out
- On average, survivors had stiffer arteries than controls, and women showed a stronger effect. In many, the change looked like five to ten extra years of “vascular age.”
- Blood pressure and markers that go with stiffness were higher for months after illness.
- Good sign: in a sub-group followed longer, stiffness stopped worsening and in some people eased a little, suggesting recovery is possible.
- Not equal for all: risk was higher with older age, high blood pressure, diabetes, kidney disease, obesity, smoking, and repeated infections.
Why this is serious even if you feel fine
- Stiffness is invisible—no fever or cough. Yet it pushes long-term risk up. If a fraction of the huge survivor population keeps this extra vessel age for years, the health-care load (clinic visits, medicines, admissions) will rise sharply—more so in countries like India, where blood pressure and diabetes are common and often detected late.
What may be happening inside the body and who must be most careful
Likely reasons
- Inflamed vessel lining (endothelium): the virus and the immune response irritate the inner wall, making vessels less elastic and more prone to clot.
- Immune “after-echo”: lingering signals keep vessels on high alert even after the virus is gone.
- Tiny clots and sticky proteins: they disturb smooth blood flow, adding stress.
- Autonomic imbalance: the body’s automatic control of heart rate and vessel tone goes off—some people feel dizzy or get a racing heart on standing.
- Indirect strain: less activity during illness, poor sleep, anxiety, and weight gain worsen sugar and pressure control.
Higher-risk groups
- Age over 50
- Women with past blood pressure, diabetes, or autoimmune illness
- People who had severe COVID or repeated infections
- Those with kidney disease, obesity, or smoking history
Red flags that need a check
- New or lasting chest pressure, breathlessness, or unusual tiredness
- Palpitations, light-headedness, or near-fainting on standing
- Repeated home blood pressure above 140/90
- Leg swelling, sudden weight gain, or much less urine
- Stroke-like signs (severe headache, face or arm weakness) — emergency care
Common myths, cleared in one breath
- “I am young, so safe.” — Young people can still have raised blood pressure or sugar; repeated infections add risk.
- “If I feel fine, nothing is wrong.” — Stiffness is often silent.
- “It is all anxiety.” — Studies show measurable vessel changes and rhythm shifts; mind-body care helps, but the biology is real.
- “Exercise is risky after COVID.” — Graded exercise is usually helpful after the acute phase; stop and seek care if chest pain, severe breathlessness, or fainting occurs.
How to check, manage, and recover—at home, in primary care, and in hospitals
At home (first line)
- Keep a two-week blood pressure log (morning and evening).
- Track resting pulse and daily steps; aim to return gently to pre-illness levels.
- Note triggers in a simple diary (heat, standing, poor sleep, caffeine, heavy meals).
At primary health centres
- Do basic tests: blood pressure (sitting and standing), sugar, cholesterol, kidney function; ECG for rhythm.
- Review sleep, salt intake, tobacco, alcohol, activity, weight.
- Give counselling on gradual exercise, salt control, stress care, and vaccine boosters.
At specialist clinics (if red flags or symptoms persist)
- Pulse wave velocity or similar stiffness tests (where available).
- Echo (heart ultrasound) for function and valves.
- Holter or a simple wearable to capture heart-rate swings and fast pulse on standing.
- Exercise test when safe, to document effort tolerance and blood pressure response.
- Inflammation or clot markers when required.
What usually helps (simple, proven)
- Walk most days. Start short, add minutes weekly; try 3 minutes easy + 1 minute brisk cycles.
- Strength twice a week with light resistance to improve glucose and vessel health.
- Less salt and packaged food; home cooking with herbs and lemon for flavour.
- Sleep 7–8 hours, cool and dark room, limit screens at night.
- Breathing and stress tools (slow nasal inhale, longer exhale; yoga or meditation).
- No tobacco; cautious alcohol.
- Vaccination reduces severe reinfection and indirect heart strain.
When medicines enter
Doctors may start or adjust blood pressure drugs, statins, sugar medicines, or a beta-blocker for fast heart rate. Avoid self-medication; doses must match the person, especially when standing blood pressure drops easily after illness.
What India can do now
Screen early, screen widely
- Add a post-COVID heart check to routine primary care: blood pressure, sugar, weight, and a three-question symptom screen.
- Run mobile camps in urban slums and remote blocks with quick blood pressure, sugar, ECG, and a clear referral path.
Put women at the centre
- Train staff to catch atypical symptoms in women (fatigue, breathlessness, jaw or back ache).
- Pair heart checks with women’s visits (antenatal, postnatal, family planning, anaemia clinics).
Heat and air plans as health plans
- Alert citizens on very hot or bad-air days: hydrate, avoid hard outdoor work, keep homes cool, use good masks in dusty air.
- Expand cool roofs, shade, and drainage to cut daily triggers of heart stress.
Make clinics resilient
- Shade and cool waiting areas, safe drinking water, clear heat-wave protocols, and backup power for vaccine fridges and oxygen.
Build usable data
- Set up a simple district registry for post-COVID cardiovascular outcomes: blood pressure control, hospitalisations, deaths, and recovery.
- Publish monthly dashboards so states copy what works (for example, districts that improved blood pressure control after extra community follow-up).
Equity and trust
- Reach the poor first; stiff arteries are silent and missed where checks are rare.
- Protect data privacy while tracking outcomes.
- Communicate support, not blame; many saw sugar, weight, and pressure worsen during lockdowns and illness.
COVID left visible lung scars in some and invisible vessel scars in others. The vessel scars show up as stiffer arteries, a slow driver of future heart, brain, and kidney disease—especially in women and people with blood pressure or diabetes. The response is practical and affordable: early screening, steady follow-up, women-centred care, cool and clean cities, and simple public dashboards. This is low-cost medicine with a very high return.
Exam hook
COVID’s most expensive legacy may be “silent” vascular ageing. If recovered adults carry arteries acting five to ten years older, the lifetime risk of stroke, heart failure, kidney strain, and dementia will rise. The fix is basic but powerful: check early, move daily, cool cities, clean air, protect clinics, and track outcomes.
Key takeaways
- Recovered people—especially women—often show stiffer arteries equal to five to ten extra years of vascular age.
- Stiffness is silent but raises long-term risk of stroke, heart attack, kidney disease, and memory decline.
- Risk climbs with age, hypertension, diabetes, kidney disease, obesity, smoking, and repeat infections.
- Home logs, basic clinic tests, and graded activity catch problems early and aid recovery.
- Policy must merge health with city design: heat safety, clean air, shaded streets, cool roofs, and resilient clinics.
- Keep a women-first lens and publish simple dashboards so districts learn and improve.
UPSC Mains question
Question:
“Recent multinational evidence suggests COVID survivors show higher arterial stiffness—akin to five to ten extra years of vascular age—especially among women. Discuss the public-health implications for India and design a district-level package to detect and reduce this risk.”
Hints to structure: define arterial stiffness and how it is measured → list high-risk groups and likely mechanisms (endothelium, inflammation, autonomic imbalance) → give a three-tier action plan (home logs; primary care checks; referral tests and medicines) → link with heat and air-quality measures → add women-centred steps and a simple data dashboard → short conclusion.
One-line wrap
Treat COVID’s quiet legacy with loud basics—test early, move daily, cool and clean our cities, and put women at the centre—so tomorrow’s hearts do not pay for yesterday’s virus.
Share This Story, Choose Your Platform!
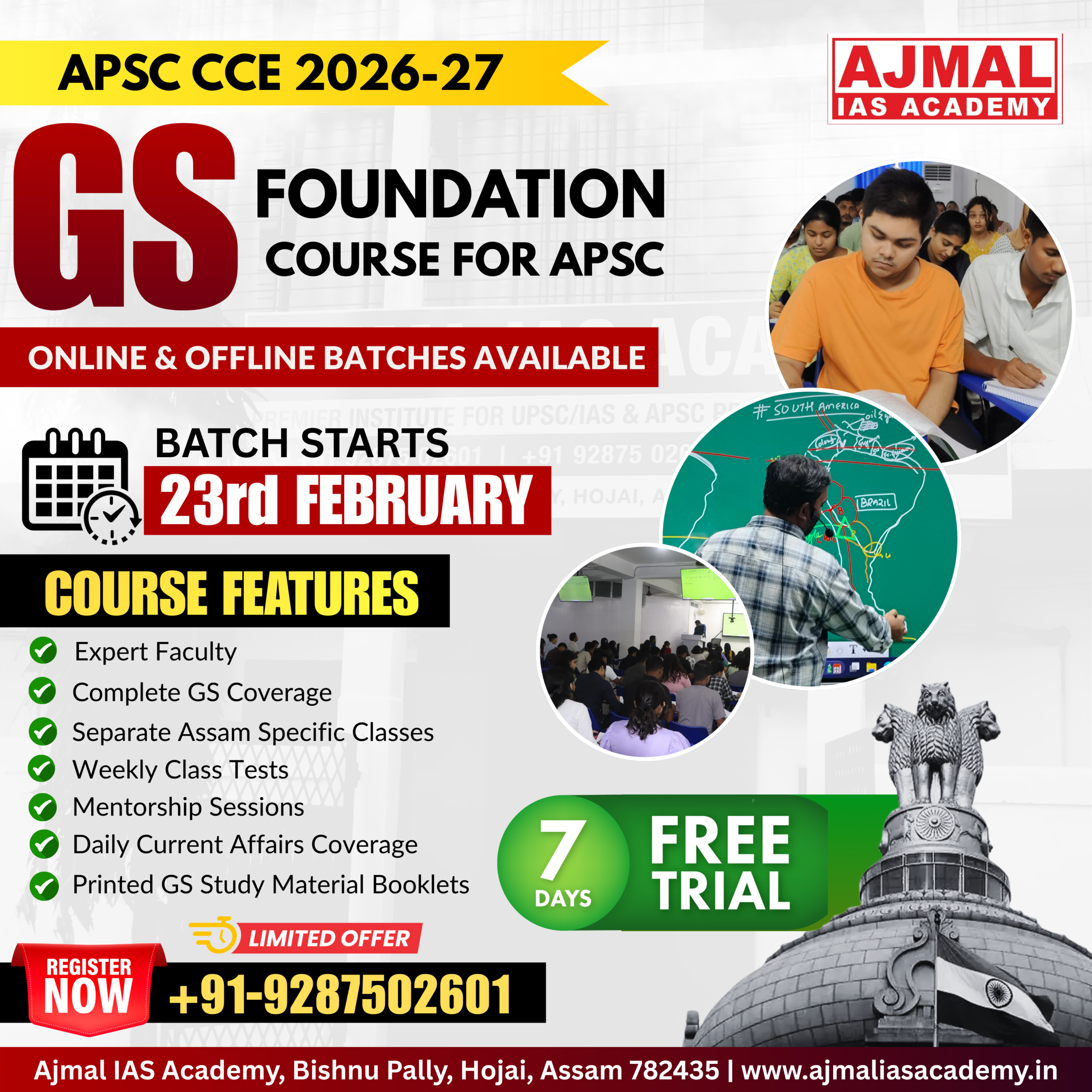
Start Yours at Ajmal IAS – with Mentorship StrategyDisciplineClarityResults that Drives Success
Your dream deserves this moment — begin it here.