Syllabus: GS-II & V: Governance & Social Justice: Health policy, rights-based approaches, mental health services.
Why in the News?
Every year on October 10, the world observes World Mental Health Day. The 2025 theme is “Mental Health in Humanitarian Emergencies: Access to Services in Catastrophes and Crises”, highlighting the urgent need to provide psychological care during disasters, crises, and beyond.
Recently, the unexpected death of cultural icon Zubeen Garg in Assam triggered widespread grief, despair, and even suicide attempts among fans. His loss demonstrates that mental health emergencies are not limited to natural disasters or pandemics — emotional shocks from the death of a revered figure can precipitate a broader psychosocial crisis. In contexts like Assam, where mental health infrastructure is limited and stigma remains, this emphasizes the necessity of integrating mental health services into crisis response frameworks.
Concern: Mental Health Issues among the New Generation
- Young people — especially aged 18–25 — are facing high academic stress, unemployment, social media pressures, and uncertainty, making them vulnerable to anxiety, depression, substance abuse, and suicidal tendencies.
- In Assam and Northeast India, gaps in counselling services, awareness, and support systems worsen the situation.
- The Supreme Court has observed that rising student suicides reflect systemic failures in addressing mental health.
- Experts have noted that stigma prevents many from seeking help early, leading to deeper complications.
Status of Mental Health in India
National Overview
- In 2017, an estimated 197.3 million Indians had some form of mental disorder — roughly 14.3% of the population.
- The National Mental Health Survey reported 5.1% prevalence for common mental disorders (depression, anxiety) with a treatment gap of about 80%.
- The suicide rate in India in 2022 was 11.6 per 100,000 population.
- India’s health budget allocation to mental health remains minimal — around 0.06% of total health expenditure.
- The mental health workforce is critically low, with only about 0.3 psychiatrists per 100,000 people compared to global standards.
Assam / Northeast Perspective
- Assam runs the District Mental Health Programme under the National Mental Health Programme (NMHP), but it is not present in all districts; those where it functions face staff, medicine, and funding shortages.
- A study covering districts of Assam shows significant variation in prevalence and uptake of mental health services across regions.
- During the COVID-19 pandemic, Assam launched “Monon: Assam Cares” as a mental health initiative to provide remote counselling support.
- Assam’s health department aims to reduce stigma and expand mental health services in district hospitals and medical colleges.
Challenges in Mental Healthcare in India
- Huge Treatment Gap & Low Service Utilization: Many persons with mental illness never access care due to stigma, lack of awareness, or inability to pay.
- Scarce Human Resources & Infrastructure
- Very few psychiatrists, psychologists, and psychiatric nurses.
- Overburdened tertiary centres and lack of community mental health facilities.
- Budget Constraints & Low Funding Priority: Mental health remains under-funded; allocation is often less than 1% of health budgets.
- Stigma, Cultural Beliefs & Social Barriers: Myths, discrimination, and shame prevent people from seeking help.
- Poor Integration with Primary Healthcare: Mental health is not yet mainstreamed into primary health systems, limiting early detection.
- Lack of Crisis Response in Events & Disasters: In emergencies (natural or emotional), there is limited capacity for Psychological First Aid (PFA), trauma counselling, or helplines.
- Uneven Regional Access: States like Assam have sparse coverage; rural and remote areas remain underserved.
- Data Gaps & Monitoring Issues: Inadequate data at state/district levels hampers effective resource allocation.
- Continuity of Care & Long-Term Support: Even when care starts, follow-up, rehabilitation, and social reintegration are weak.
Government Initiatives & Policy Frameworks
- Mental Healthcare Act, 2017: Guarantees the right to access mental health care, decriminalizes suicide, and ensures informed consent and protection of rights.
- National Mental Health Programme (NMHP): Launched in 1982 to integrate mental health into general healthcare and provide district-level services.
- Tele-MANAS / Tele-Mental Health Helplines: A national tele–mental health network providing remote counselling and crisis intervention through a toll-free number (14416).
- Health & Wellness Centres (under Ayushman Bharat): Include mental health screening and referral functions.
- National Suicide Prevention Strategy: A comprehensive plan to reduce suicides through coordinated, multi-sectoral actions.
- Digital Mental Health Platforms & Innovation: Use of telemedicine, online counselling, and mobile apps for mental health support.
- State-Level Programmes: Assam’s District Mental Health Programme and Monon: Assam Cares integrate counselling in district hospitals.
- Civil Society & NGO Efforts: Community-based mental health initiatives, awareness campaigns, and peer support networks led by NGOs.
Way Forward
- Strengthen Primary & Community-Based Mental Health Services: Train and deploy lay counsellors in villages and integrate mental health into ASHA and primary care networks.
- Emergency & Crisis Response Integration: Include mental health modules in disaster management plans, deploy Psychological First Aid, activate crisis helplines after major emotional or cultural events, and ensure continuity of services.
- Capacity Building & Workforce Expansion: Expand psychiatry training seats, incentivize rural practice, and recruit psychologists and social workers.
- Increase Budget Allocation: Raise mental health funding to at least 1-2% of health budgets and allocate dedicated funds for counselling and infrastructure.
- Stigma Reduction & Awareness Campaigns: Use media, schools, and workplaces to normalize mental health discussions and promote early help-seeking.
- Digital & Hybrid Innovations: Leverage tele-mental health, mobile counselling apps, and culturally adaptive digital platforms for adolescents.
- Data & Monitoring Systems: Create state and district-level databases to track prevalence, service delivery, and outcomes.
- Follow-up & Rehabilitation Support: Link patients to community rehabilitation, social support groups, and livelihood programmes.
- Cultural Integration & Local Coping Mechanisms: In Assam and other regions, integrate music, cultural rituals, and community gatherings into therapeutic processes.
- After emotional events like the Zubeen tragedy, deploy culturally sensitive grief counselling.
- Media Responsibility: Avoid sensational coverage of suicides or tragedies; focus on helplines, recovery stories, and coping resources.
Conclusion
Mental health is central to human dignity, social cohesion, and resilience. Despite growing recognition, India’s mental health system faces deep structural and cultural challenges. Events like the death of Zubeen Garg highlight that mental health emergencies can be cultural and emotional, not just medical or natural.
By integrating mental health into primary care, disaster management, education, and culture, expanding the workforce, and eradicating stigma, India — and particularly states like Assam — can make mental healthcare truly inclusive and accessible. The 2025 theme reminds us that mental health must be at the heart of all crisis response and recovery frameworks.
Mains Question
“In light of the 2025 World Mental Health Day theme — ‘Mental Health in Humanitarian Emergencies’ — critically discuss the challenges and strategies for ensuring access to mental health services in India, particularly in states like Assam.”
Share This Story, Choose Your Platform!
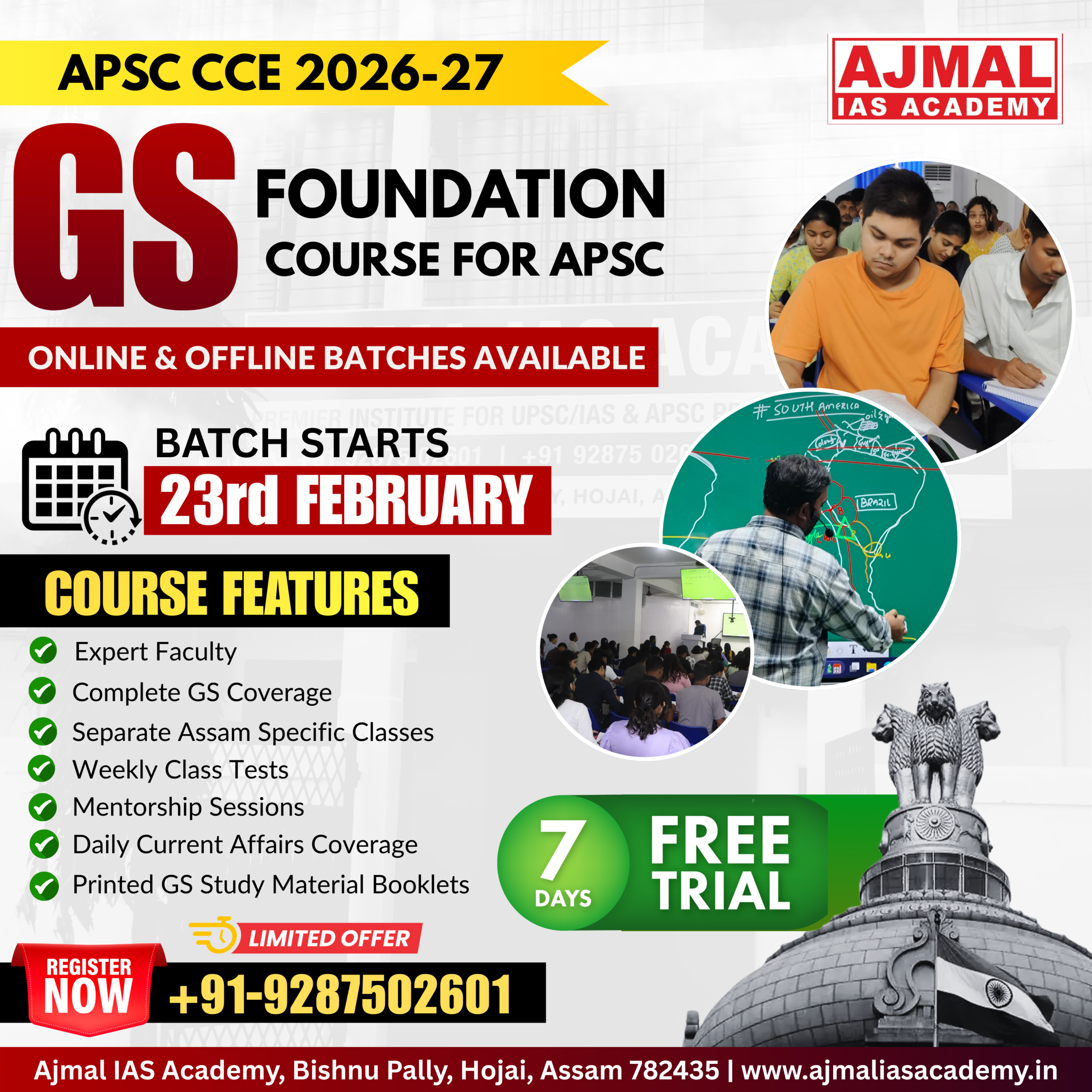
Start Yours at Ajmal IAS – with Mentorship StrategyDisciplineClarityResults that Drives Success
Your dream deserves this moment — begin it here.